Doctors and engineers have begun to combine their strengths, and new professions and innovative therapies have come out of it.
When Idris Guessous talks about his work group, he often compares it to a family. “When the GIRAPH (Geographic Information Research and Analysis in Public Health) programme was launched in 2013, my colleague Stéphane Joost and I formed a team of scientists,” says the physician and epidemiologist. “The family then grew and now includes children and friends who are our students and employees.” What’s special about this two-man team? One is a registered physician with the Lausanne University Medical Polyclinic (read the portrait p. 15), and the other is specialised in geographical information systems at EPFL.
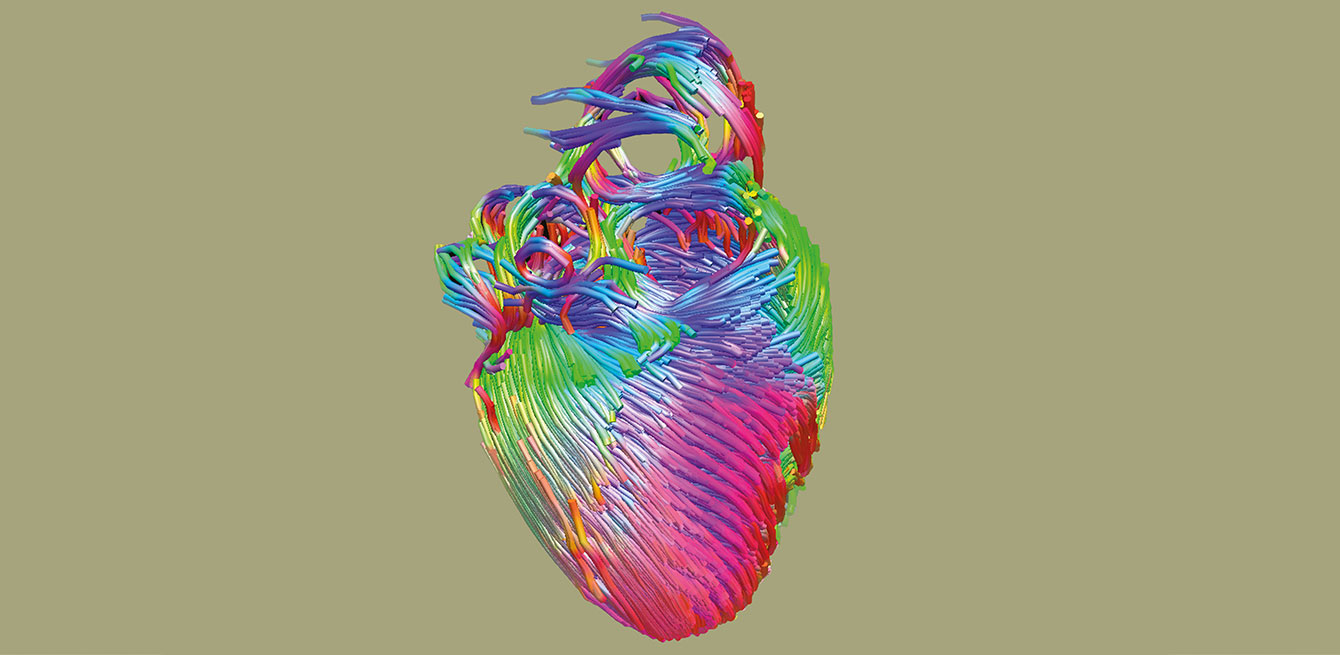
This example is not a one-off incident. These days, medicine and engineering are increasingly fused to bring about innovation. Piergiorgio Tozzi, an associate physician with the Cardiac Surgery Service at Lausanne University Hospital (CHUV), has been working with engineers for 18 years. Together, they designed a medical device to improve the surgical treatment of mitral insufficiency. This little valve in the heart prevents blood from flowing back from the left ventricle into the left atrium. After four years of development, the medical practitioner hopes to implant the device in a patient for the first time this year.
1 / Speaking two different languages
Certain ingredients have to be added for the blend to work. “Passion, curiosity and an open mind,” Piergiorgio Tozzi says. That doesn’t mean that everything will go smoothly. As the cardiac surgeon says, “Engineers and doctors speak two different languages. Engineers are used to precision and certainty, while doctors have to deal with a lot of surprises.” This difference can complicate things, at least at first. But it’s easy to work around. “We just have to be patient and diplomatic,” the expert says with a smile.
Having worked in both fields, Jacques Fellay admits there is “a natural gap between medicine and engineering. But we now need to bridge that gap, given everything patients have to gain. Major innovations will develop from these partnerships.” As a genomics researcher at EPFL, Fellay holds a central role in this alliance. He studied infectious diseases and came to EPFL in 2011. He is in direct contact with scientific and IT engineers. Together, they hope to map out the human genome to determine whether differences influence the body’s response to infections. Today, he spends 10% of his time at CHUV, as a way of keeping one foot in both worlds. Jacques Fellay conducts what is called “translational” research, i.e. transforming laboratory discoveries into concrete applications that benefit patients.
The cardiac surgeon Piergiorgio Tozzi very clearly says that his field of science can’t do without this collaboration. “When doctors detect a problem ‘in the field’ they can ask engineers for help to develop a solution.” This offers a dual advantage. Practitioners give engineers an idea, and they put it into application. “They actually find it very rewarding to work on health data,” says the epidemiologist Idris Guessous.
2/ Not just for doctors
Most of the time, this type of cooperation comes about by chance. Doctors and engineers are brought together at seminars or study-abroad programmes. In the United States especially, medical students do translational research and dissertation work right at clinical facilities and realise that synergies exist between the two fields. Some doctors may also be approached directly by engineers looking for a clinical application for their product.
That’s what happened to the ergotherapist Julien Moncharmont, who was contacted by Andrea Biasiucci, a biomedical engineer and co-founder of the EPFL spin-off Intento. Together, they developed technology for functional electrical stimulation aimed at hemiplegic patients. “Electrodes placed on the arm create a series of contractions that reproduce the functional movement of the limb, such as picking up or setting down a glass,” Moncharmont explains. “This technique brings hope for patients with chronic hemiparesis to be able to move their arm and use it in daily living activities.” An experimental project was conducted on about 12 patients in the autumn of 2015, producing conclusive results.
3/ Rapid expansion
Although the collaborative efforts between medicine, health care and engineering are growing fast, they’re nothing new. “Back in ancient times, technicians would use engineering principles to develop processes that could be used in medicine, such as orthopaedic implants,” says Vincent Barras, medical historian at CHUV. “But it wasn’t until the late 19th century that this type of cooperation became clear. Doctors would seek out engineering staff to develop new techniques.” For example, radiologists have been working with physicists since 1899, when X-rays were discovered. These non-medical experts are responsible for the technical aspects concerning the production and use of ionising radiation to ensure the safety of patients and health care staff. “Interaction between the two fields is becoming more widespread,” Fellay says.
The new experts emerging from the combination of technology and medicine will become as essential as general practitioners. “Bioengineers and bioinformaticians will soon play a key role in our health system,” says Fellay. Researchers and practitioners need to work more closely together than ever, as new technologies change the way doctors work. Some teams, including the one overseen by the epidemiologist Idris Guessous, have already brought in programmers or digital health specialists. /
Promoting partnerships
The Swiss National Science Foundation (SNSF) set up the research programme Sinergia to support interdisciplinary cooperation. The SNSF financed 42 new Sinergia projects in 2015, for a total of 63.8 million Swiss francs. Out of the 126 requests for funding submitted, 26% of the projects were related to mathematics, natural sciences and engineering, while 54% involved biology
and medicine.
Higher education also emphasises this fusing of scientific expertise. Schools in Basel, Ticino and Zurich have even teamed up to offer a new medical studies programme in 2017. Students who complete their bachelor’s degree at the Swiss Federal Institute of Technology in Zurich can do their master’s in medicine at one of the partner universities. They can specialise in areas such as medical information technology or biomedical imaging. The University of Lausanne (UNIL) began to offer crossover programmes combining biology and bioengineering with medicine in 2012. “We want to strengthen that approach,” says Giorgio Zanetti, director of the medical school at UNIL, “to better integrate the expertise we need.”
In Lausanne, many bridges have been built between the university hospital and the polytechnic school:
434
scientific studies by researchers from the two institutions have
been published between
2011 and 2015.
/
18
patents were filed in 2015
by EPFL’s Faculty of Life Sciences.
5 start-ups were founded
and 7 licences granted.
/
1,007
students were enrolled at
the Faculty of Life Sciences
at EPFL in 2015. That number
was 364 in 2005.
/
300
million Swiss francs will be
donated over the next 30 years
to the Ludwig Center for Cancer Research in Lausanne. CHUV,
EPFL and UNIL all work together
at this centre to conduct
anti-cancer research.