
COVID-19 has brought viruses into the conversation like no other event before it. With their amazing ability to adapt, viruses have taken over the planet. But humans have also had to adapt by studying viruses to protect themselves. Here is an overview of the large family of viruses.
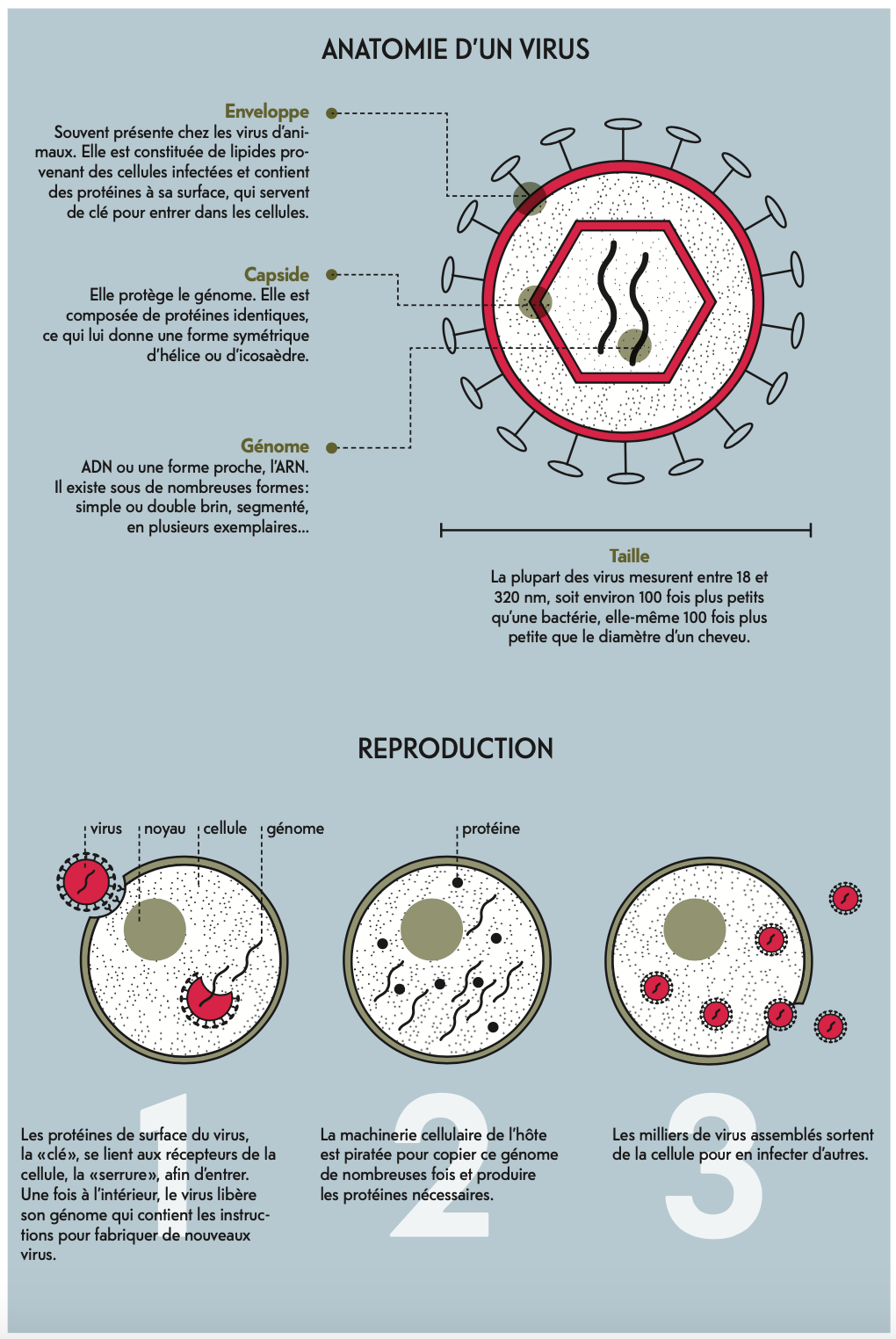
In the kingdom of living things, viruses are often set into a class of their own. They resemble no other known forms of life on Earth, all of which are made up of one or more cells. Viruses are made up only of a genome, enveloped in a capsule of proteins and sometimes lipids. As they have no cell structure, they have to find cells to multiply. That is why some scientists do not consider them to be alive. Meanwhile, others believe that their complexity and ability to adapt and evolve make them living organisms. Perhaps they are but merely transitory beings. Some theories suggest that viruses appeared before other forms of life, or used to be living organisms that lost most of their cellular functions.
Living or not, viruses are diverse and found everywhere, in water, in the air, in the soil. They infect all forms of life: bacteria, plants, insects, humans, and even one another. Today, more than 5,000 species of viruses have been identified, but there are probably millions of them. Among them is the famous Coronaviridae family, which includes four species of seasonal coronaviruses that cause colds (CoV) and three more virulent species that cause “severe acute respiratory syndrome” (SARS). These three are: SARS-CoV-1, which caused an outbreak that started in China and lasted for two years; SARS-CoV-2, responsible for the COVID-19 (coronavirus disease 2019) pandemic; and MERS-CoV, which originated and is still present in the Middle East.
Other families include human influenza viruses and haemorrhagic viruses such as Ebola. Phages are viruses that mainly infect bacteria and are also classified into different families. Then there are “giant” viruses, such as the mimivirus. They were discovered in an amoeba, their host, and were first mistaken for a bacterium due to their gigantic size. Their genome can contain over 1,000 genes, much more than other viruses and some bacteria. These characteristics challenge traditional definitions of viruses and their place in the tree of life.
One of the key ways viruses adapt is by mutating. While viruses replicate in infected cells, small changes can occur in the viral genome due to copying errors called mutations. While most of these mutations either have no effect on or harm viruses, mutations that give them an advantage will be retained by natural selection. These mutations can allow viruses to infect their host in a highly targeted manner, cross the species barrier, evade the immune system, or resist treatment and vaccines. For SARS-CoV-2, whose primary host was likely a bat, mutations favoured its adaptation to human cell receptors and probably its ability to infect and cause disease. Since then, new mutations have appeared, especially in genes encoding the spike protein, the “key” to entering cells. These variants, which appeared in the United Kingdom, South Africa and Brazil, seem to spread more rapidly than the original variant.
Influenza viruses also adapt through mutations. They remain infectious by frequently changing their antigens, molecules that trigger the immune response. That is why new vaccines are created every year, to adapt to antigenic variation. But sometimes a much more abrupt change occurs in flu viruses. When two different viruses infect the same cell, they can exchange gene fragments and create a new genetic combination. As a result, a new virus emerges, going unrecognised by the immune system. “These new gene sequences are what causes major flu epidemics,” says Gilbert Greub, director of the Institute of Microbiology at the University of Lausanne and physician in chief of the diagnostic microbiology laboratories at Lausanne University Hospital (CHUV). “The Spanish flu in 1918 caused between 25 million and 100 million deaths worldwide. In 1956, there was the Asian flu, and in 1968 a new combination with fragments of avian virus brought about the Hong Kong flu.” Closer to our times, avian flu broke out in 1997 and 2003, and swine flu in 2010, containing fragments of avian, swine and human viruses.
Some viruses use the hit and run strategy to survive. They multiply very quickly and destroy the cell, causing severe inflammation. They must then escape and find a new host before they are attacked by the immune system or the host dies. Viruses do that via the respiratory tract, as for coronavirus, influenza and measles; animal bites for rabies; or secretions for Ebola. Infection is therefore highly transmissible and acute, which means rapid onset of symptoms.
Alternatively, hit-and-stay viruses strike less hard... but linger. The virus persists in the host’s cells, latent, without multiplying, sometimes integrating into the genome. In this case, the virus must find a balance between being overly virulent and killing the host, and remaining discreet enough to survive, undetected by the immune system. However, over its lifetime the virus can reactivate. This is why herpes reactivates when our immunity drops, causing cold sores. The chickenpox virus can also reactivate years later and cause shingles. This type of infection is therefore chronic (long-lasting) with little or no transmission during the latency period.
Another factor to consider in an infection is contagiousness, i.e. a measure of how easily the virus is transmitted. This mainly depends on the total viral load (the number of viruses in the host), the viability of the virus outside the host, its ability to enter the host, and the mode of transmission. “Contagiousness is measured in terms of R0, or reproduction number, which refers to the number of people that the virus contaminates if nothing is done to prevent it,” says Gilbert Greub. “SARS-CoV-2 has an R0 of about 3, so an infected person can transmit the disease to an average of three other people.” As a comparison, measles has an R0 of 12, and seasonal influenza 1.5. Fortunately, we can do things to help lower the effective reproduction number, or Re, of the virus. Preventive measures taken for COVID-19 – such as social distancing, washing hands, or wearing a mask – reduce the risk of spreading the virus. When the Re falls below 1, it means that the number of new infections decreases. Although out of our control, another factor that can alter contagiousness is the seasons. In summer, SARS-CoV-2 has a lower Re because it is less viable in warm, humid air. We also spend more time outdoors, while the opposite is true in winter.
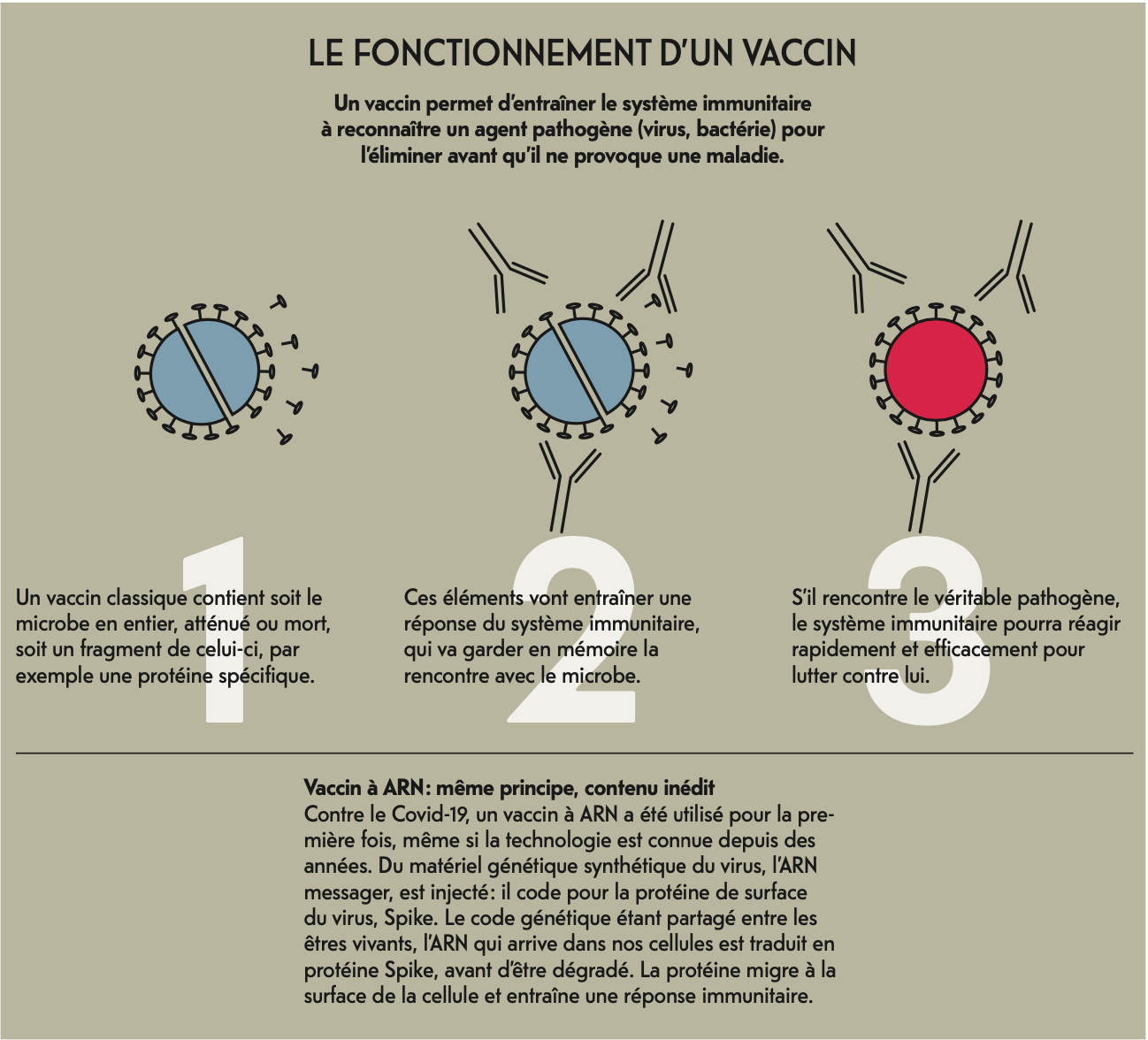
We have learnt to live with many viruses and adapt to them, such as the flu, Gilbert Greub points out. “We generally suffer from it from childhood without too many problems, and vaccines exist to protect people at risk. We will probably have to live with SARS-CoV-2 as well, trying to contain it and have a vaccine for those at risk. And vaccines will have to adjust to the evolution of the virus and the variants circulating.” So far, only one disease caused by a virus has been eradicated: smallpox, back in 1980. However, stocks of the virus are still kept for research in two high-containment laboratories. Polio is on the same path. The virus was declared eradicated in Africa in August 2020 by the World Health Organization and only remains in Pakistan and Afghanistan. For all others, we have had no choice but to adapt by developing preventive measures, vaccines and treatments to limit the spread and effects of the disease.
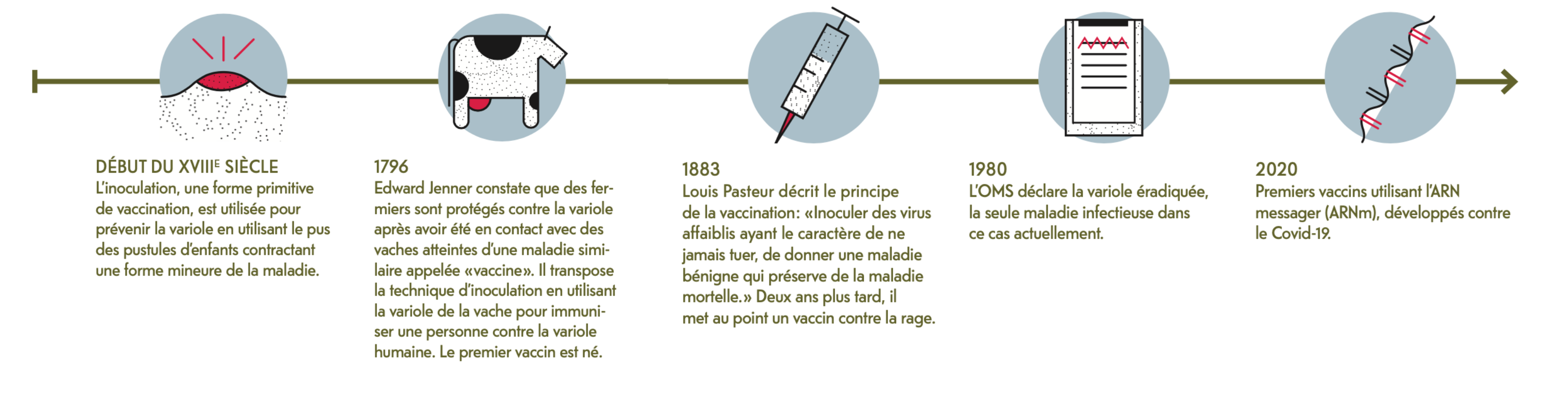
Early 18th century
Inoculation, an early form of vaccination, is practised to prevent smallpox, using the pus from pustules on children who had contracted a less severe form of the disease.
1796
Edward Jenner finds that farming communities are protected against smallpox from their contact with cows infected with a similar disease, cowpox. He transposed the inoculation technique by using cowpox to immunise an individual against human smallpox. The first vaccine was created.
1883
Louis Pasteur describes the principle of vaccination as inoculating weak forms of viruses with the character of never killing, giving a benign disease that protects against the deadly disease. Two years later, he developed a vaccine against rabies.
1980
The WHO declares smallpox, the only infectious disease of its kind today, eradicated.
2020
First vaccines using messenger RNA (mRNA) are developed against Covid-19.
Reconstructing the virus in Bern
In February 2020, laboratory scientists at the University of Bern cloned the coronavirus (SARS-CoV-2). This research is crucial. Reconstructions of poliovirus, Spanish flu virus and more recently Zika have helped us better understand their virulence and provided clues towards potential treatment and prevention solutions for current and future pandemics.
To reconstruct the virus, researchers at the Institutes of Veterinary Bacteriology used yeast-based synthetic DNA fragments to reassemble the complete virus genome. Early in the pandemic, this method enabled research groups around the world to study the virus before they even had access to samples from infected patients.
The method also makes it possible to study mutated virus strains circulating in the population without having to wait for new samples. “We can recreate all the mutations of the variant we want in vitro under controlled conditions,” says Fabien Labroussaa, a veterinary bacteriology researcher at the University of Bern. “This gives us insight into the impact of a mutation on virus behaviour and lets us compare various strains. We can also add fluorescent markers to test antiviral compounds more quickly.”
When the whole virus is not available, scientists can study fragments of its genome, such as the spike protein coding gene. This approach can be used to develop new RNA vaccines. “This protocol is fast, but it can’t be used to study the complete biology of a virus, such as how it replicates and is transmitted in vivo.”
What about the dangers? Research on synthetic viruses is highly regulated and requires authorisations. The final step of infecting cells, which allows the virus to replicate, is conducted exclusively at the high-security laboratory in Mittelhäusern near Bern. “The risk of the virus escaping is close to zero because of the equipment and measures in place.” As for the risk of the system being used as a biological weapon, Labroussaa points to the notion of dual-use goods in science. On one hand, major discoveries advance science, while on the other, they can be misused. A frequently cited example of this is nuclear energy. “In itself, our technique is highly controlled, and it would be complicated for anyone without special equipment or knowledge.”
How was it possible to eradicate smallpox, unlike other viruses? First, smallpox had only one reservoir, meaning that the virus only multiplied in humans. SARS-CoV-2, on the other hand, has several reservoirs (bats and pangolin), which increases the chances that it will re-emerge and infect humans. Second, smallpox had the distinctive, easily detectable symptom of pustules all over the body. In contrast, the symptoms of COVID-19 (coughing, fever) are not unique to this disease, making it difficult to identify. Plus, about one-third of those infected are asymptomatic. For HIV, initial symptoms only appear after a long latency period, so the virus can be transmitted while it is undetectable. Also, HIV infection is chronic, which makes it more difficult to eradicate. Another key factor is the stability of the virus genome. For example, DNA viruses, such as smallpox, are very stable, while RNA viruses like HIV mutate rapidly, which makes it difficult to develop a vaccine. “At a more general level, eradicating a virus requires a collective effort, political support and geopolitical stability, especially to conduct globally coordinated vaccination programmes.”
The current impacts of COVID-19 on research, clinical practices and society could last longer and be expanded, says Oriol Manuel, senior physician at the Infectious Diseases Service and Centre for Organ Transplantation at CHUV. “We have understood the need for a strong public health system and the importance of scientific research and collaboration. We will therefore watch this type of virus more closely to control it earlier.” The innovative research that led to the SARS-CoV-2 vaccines could also serve as a platform for developing new vaccines against influenza and other respiratory viruses.
The multi-centric clinical studies that have proven useful in testing COVID-19 therapies can also apply effectively to other situations. They involve large numbers of patients and are conducted using the same protocol in different countries at the same time. In hospitals, staff will probably continue social distancing and wearing masks when in contact with patients to prevent contagion of other respiratory or influenza viruses. In society too. “People at risk might continue to wear masks, but they will no longer be stigmatised for it.”
About 200 species of viruses are capable of infecting us. That is only a handful of the thousands, if not millions, that exist, but they capture our attention because of the diseases they can cause. However, viruses are much more than pathogens, and some are beneficial to humans. They are part of our intestinal microbiota, although their role remains poorly understood. Most of them are phages, viruses that infect bacteria. Phages can be used as a therapy to fight bacterial infections, which is useful when dealing with antibiotic resistance. Plus, phages have the potential to target only certain pathogenic bacteria, while antibiotics also kill useful bacteria.
Some viruses play an important role in the evolution of species, such as retroviruses, which integrate into the host genome. When this happens in a reproductive cell, the viral genome can be passed on to descendants. This suggests that 8% of our genetic make-up comes from retroviruses. Some sequences have become vital, and research suggests that the placenta in mammals like ourselves originally evolved from a retrovirus.
Other viruses could have beneficial effects against infections or diseases. Totally benign, pegivirus appears to offer some protection in individuals co-infected with HIV or Ebola. Experiments on mice have also shown that herpes viruses protect rodents against bacteria causing the bubonic plague and listeriosis. More recently, scientists have discovered oncolytic viruses, which can destroy cancer cells with potential to be used in cancer therapy.
On a global scale, viruses play an important role in supporting ecosystems and biodiversity. For example, phages control the microbial population in the oceans, which comprises 90% of their biomass. By destroying bacteria, phages are responsible for the life cycle that provides the nutrients necessary for phytoplankton, which produce half of the oxygen we breathe.
Threatening. Useful. Mysterious. Viruses are present in the Earth’s smallest recesses and are part of ecosystems. Today, we only know about a fraction of their tremendous diversity. But through research, we can find out how to protect ourselves from deadly viruses, prevent them from emerging and harness the power of those that could be beneficial to us. /
20 million
Conservative estimate of the number of deaths.
/
High estimate of the number of deaths, according to recent studies.
/
Percentage of the world’s population that lost their lives, based on the high estimate.
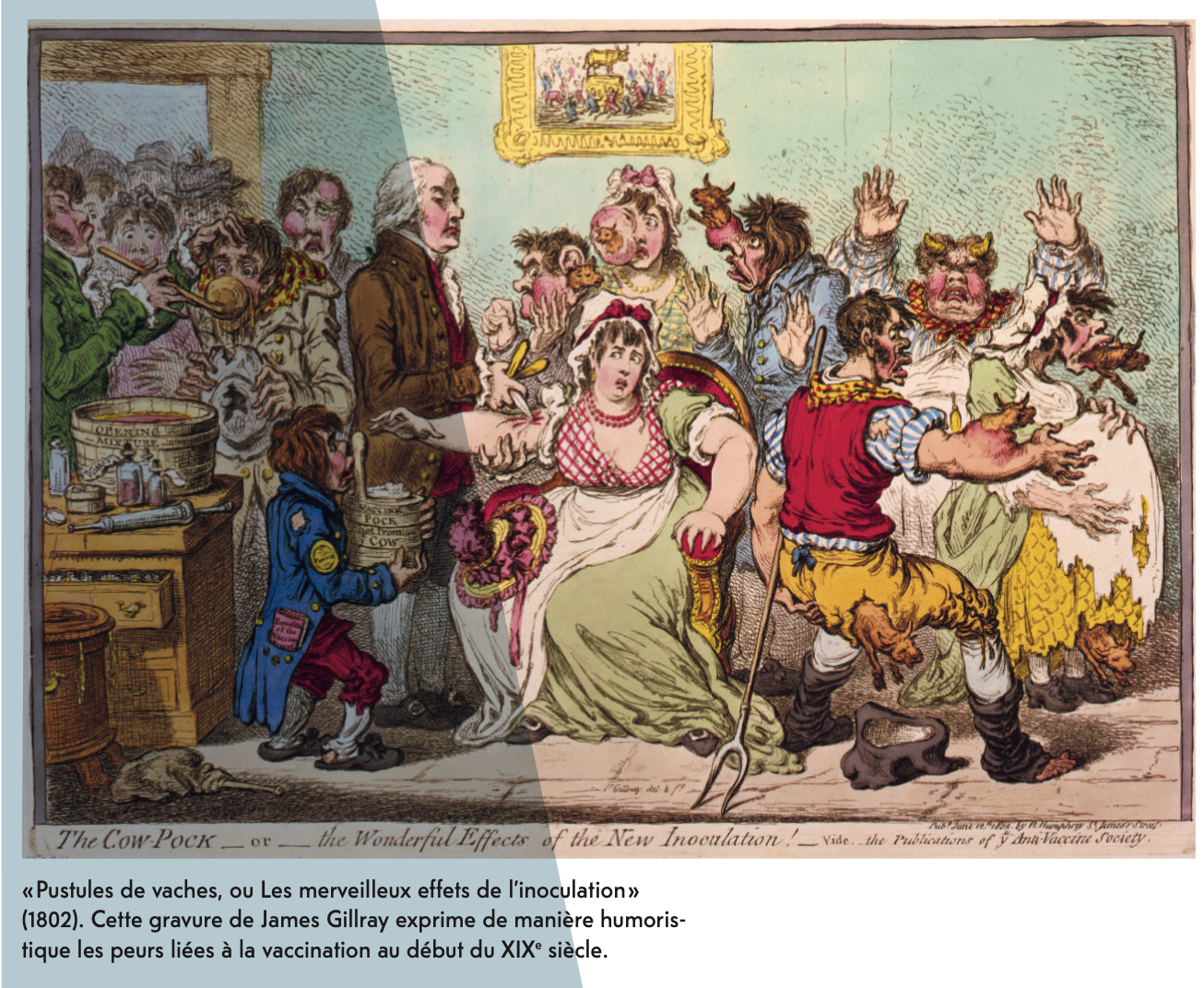
Nearly 24% of the Swiss population have said that they do not want to be vaccinated against COVID-19 in an SSR survey taken in January 2021. This scepticism is not new, as Vincent Barras, director of the CHUV-UNIL Institute of Humanities in Medicine, explains. “In the early 18th century, people argued over statistics and effectiveness of inoculation, especially in educated circles. Plus, that meant injecting oneself with variola while in good health...”
One of the key arguments supported by vaccine sceptics is the fear of making oneself sick. Another is the idea of injecting foreign matter – in the case of Jenner’s vaccine, the cow (see opposite, infographic). Western societies are also very individualistic. “Getting vaccinated is an altruistic act. It is done not only to protect oneself, but to protect people at risk and the population at large.” High vaccination coverage
is therefore necessary to prevent further outbreaks, as is still happening with the highly contagious measles.