The psychiatrist and psychoanalyst offered In Vivo his insights about the role of empathy in hospitals. In our day and age, the fast-pace development of highly specialised medicine is bound to dehumanise patient care.
IN VIVO Are you pessimistic about empathy?
Serge tisseron / I’m against bad interpretations of empathy. For example, saying that empathy means putting yourself in someone else’s place. Let’s be modest, it’s simply not possible! And would we even want that? If so, I can’t help my patients. I want to show that empathy is much more complex than we imagine. Although it can be a quality focused on altruism and helpfulness, it can also be a weapon of manipulation. Empathy is a mental construct. I try to understand someone else’s situation based on my own interpretation and personal history.
IV As a patient, what type of care provider would you like to have?
ST A care provider that keeps me informed about the progression of my illness by giving me their time to talk about it. Progress has been made in this area, but the truth is too often announced to patients as if it’s a burden that medical staff want to get rid of. The patient won’t necessarily be less traumatised by hearing the truth. I’d also like medical professionals to be punctual. It creates anxiety when they’re late for an appointment. I can’t trust someone with the treatment if I can’t trust them to be on time.
IV CHUV has closely studied the issue of dehumanisation of medical care. What do you think?
ST The risk for the patient is not being listened to, understood or taken into consideration, or of being treated like a liver or a heart, which has been accentuated with the fragmentation of disciplines. Patients often feel they’re dealing with medical professionals who act like mechanics repairing an organ. We have a long way to go to develop more integrated medicine. Some discoveries support this shift. For example, the fact that our gut flora affects brain function might help alter that concept. It’s also important to explain to students that anxiety amplifies somatic problems, and vice versa.
IV We hear more and more about personalised medicine. What do you think of steps taken by Google and Apple to develop algorithms to better detect disease and improve care for patients?
ST It’s both a wonderful opportunity and a terrible danger. For example, if retinitis pigmentosa can be diagnosed with a smartphone, action can be taken much earlier. The problem will come when artificial intelligence can diagnose health issues and suggest customised treatment in the place of doctors. “Personalised medicine”, in referring to adapting patient treatment to their physiological or biological characteristics, will lead to huge misunderstandings. People are much more than just their biological characteristics! I see two possible outcomes. Either governments and hospitals will decide that there are fewer staff, doctors and care providers; or, the other point of view is that, through technology, doctors will be able to concentrate more on the relational side of care and better integrate the psychological implications of the illness. We can’t have a machine spitting out a piece of paper that says “when you return home, here is the advice to follow”. No one will follow it.
“The doctor treats, but it’s the patient who recovers."
IV An American study published in 2009 showed that empathy in medical students diminished drastically in the third year of medicine, precisely when they come into contact with patients. What do you think of the way doctors and healthcare professionals are trained?
ST In medicine, the main enemy of empathy is the desire to control everything and be all-powerful. It’s the idea of having total control over care pathways, controlling patients so that they recover. People have the right to decide not to be treated. And doctors often have trouble accepting that. Some doctors have a problem, not with disease but with recovery. They’ve forgotten that the doctor treats, but it’s the patient who recovers. And there are patients who don’t want to recover. And that’s their right. Medical studies exalt the curative potential of doctors. Students go through their education with the idea that, with the help of progress, they will eventually be able to cure anything. That may be the case for diseases, but not patients! We must teach medical students that some patients are truly suffering without objective causes based on our current state of knowledge. Empathy means acknowledging a person’s suffering beyond what we can do for them. Doctors and healthcare providers must also be aware of their own limitations and be modest when it comes to the services they can provide. Some patients need to put the effectiveness of the treatment into perspective to be able to accept it. We have to develop more therapeutic education and hold patients accountable about the care they are given.
IV Can the patient-actor model, as a counter-balance, prevent care from being dehumanised?
ST Empathy means acknowledging that we’re reliable human professionals and that the other human, the patient, is as reliable as we are, and we are in it together to deal with the same disease. Empathy is based on trust, mutual exchange and collaboration with the patient. Doctors are not the commanders of a treatment ship with a patient loaded like cargo.
IV How can health professionals become more empathetic?
ST By teaching them to recognize their negative emotions and express them. Patients can be difficult. We need to set up support groups and department meetings so that health professionals can talk about their negative experiences. If they can’t do that they feel guilty, not for not doing enough for a patient, but for resenting patients for not recovering. That partly explains why healthcare professionals burn out. They end up resenting patients, wear themselves out trying to treat them, not so that they recover, but to avoid being confronted with the fact that they’re tired of them. Sometimes we have to accept that we’d rather the patient died. Support systems would help bring out shameful emotions that doctors feel and work with them.
IV Have you thought of other ways of fighting the increase in burnout among medical professionals?
ST Healthcare providers often burn out due to a conflict with empathy. It’s when their working conditions force them to choose between empathy for their patients and empathy for their colleagues or the institution. Empathy isn’t just an individual thing, it’s a collective responsibility. It sometimes requires major institutional changes that free up time for patients. These days, we should avoid staff restrictions, make sure they’re paid properly and recognise the value in the work healthcare providers do, because we keep asking more of them, and they end up burning out. I also think that using exoskeletons attached to the belt to help them lift heavy loads would be useful. We should start by using them in hospitals to lift or turn over bedridden patients.
In other words, for different levels of staff to show empathy for patients, they have to be shown empathy themselves. Care was traditionally administered by nuns who didn’t look for recognition from their supervisor, but from God, which they found in prayer. Today, staff are not part of the church and need their supervisors to recognise and value their work, even in a time of economic austerity! We also need to make recreational time available within the department where people can get together and where they feel supported. This involves reinstating the importance of the feeling of belonging to a group, in order to fight burnout and recognise what makes each profession different. For example, I can’t believe that training for healthcare providers is perceived as training for medical sub-tasks. It doesn’t work that way! There’s not a more prestigious professional category, i.e. doctors, and then people below them who work with illness, i.e. nursing staff.
IV What should we do to make sure health professionals succeed in the future?
ST Require future doctors to do six months of nurse training that is integrated into their university programme. And during that training time, they should work as a team, especially with nurses. Then, in the field, everyone at all levels needs to understand that they can’t give empathy if they’re not getting any themselves. Empathy isn’t something you demand of those below you, “Be empathetic so that patients recover”. It doesn’t work that way! Showing empathy as part of the structure of an organisation means being concerned about the well-being of your team. Bosses who have teams that work well are often generous and positive, and listen to them.
IV If anything was possible, what would you do?
ST I would develop meeting times where everyone can talk about their struggles in an environment of mutual kindness. A team can’t function by only showing concern for patients’ well-being. It also has to think about its own well-being and be at peace with itself. ⁄
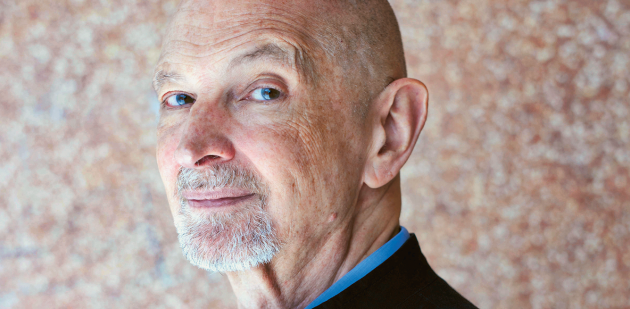
The French psychiatrist and psychoanalyst Serge Tisseron is also a researcher with the Centre for Research in Psychoanalysis, Medicine and Society at Paris Diderot University 7. His work focuses on three main areas: secrets due to trauma, relations with image and the impact of new technology on relationships with others. He is also a comic book artist and illustrator for children’s books.
“Empathie et manipulations, les pièges de la compassion”, Serge Tisseron, Albin Michel, 2017
“Le jour où mon robot m’aimera, vers l’empathie artificielle”, Serge Tisseron, Albin Michel, 2015
“Fragments d’une psychanalyse empathique”, Serge Tisseron, Albin Michel, 2013
to know more
Discover the empathy ship model developed
by Serge Tisseron on www.invivomagazine.com