Five institutions along the northern shore of Lake Geneva have launched a vast scientific cooperation programme called Health 2030. The idea is to combine their strengths and expertise to build the medicine of tomorrow.
“This project brings together 2.5 million researchers.” that’s how Professor Didier Trono, head of the laboratory of virology and genetics at the Swiss Federal Institute of Technology, likes to describe this new initiative to come out of the Lake Geneva region, Health 2030. “It’s not just scientists. It involves citizens throughout Western Switzerland.” Together, they will contribute to the development of personalised medicine. Also referred to as “precision medicine”, this approach aims to offer a more precise diagnosis and treatment customised to each patient.
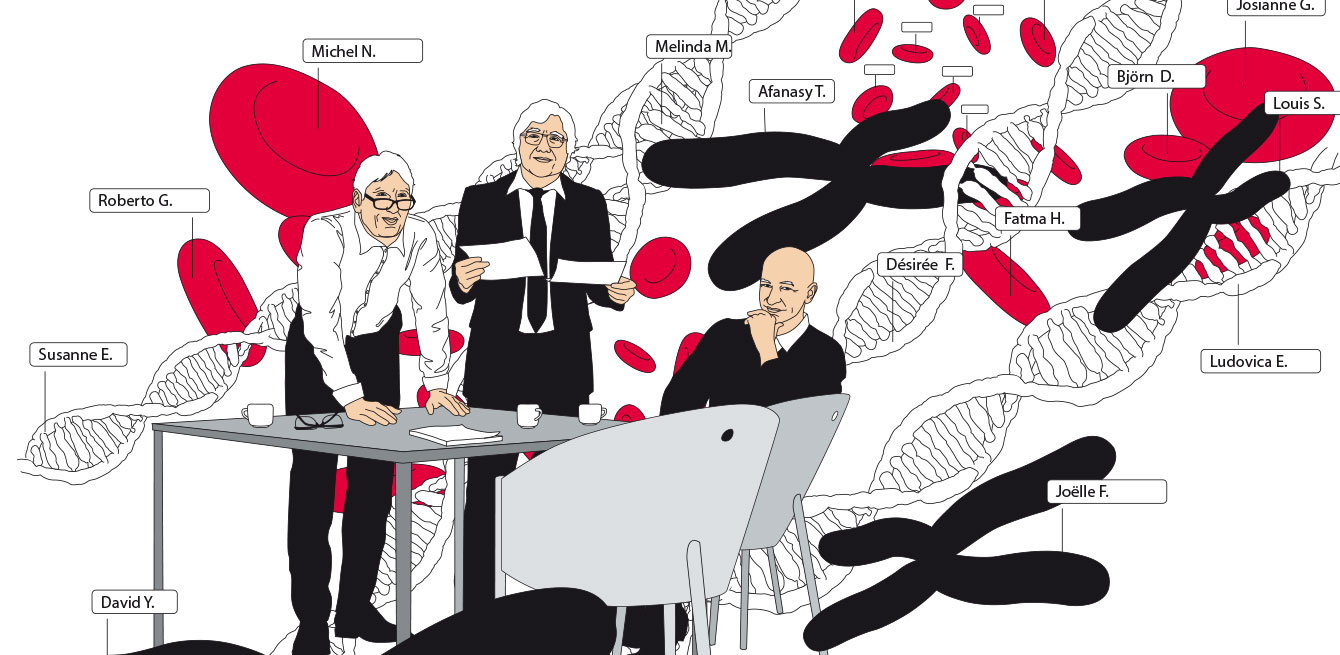
The model also emphasises the importance of prevention by identifying the risk of disease in early stages. “Personalised medicine requires considerable resources and a wide range of expertise. It won’t work at merely a regional or even national level,” says Philippe Moreillon, vice dean of the University of Lausanne. He is one of the three members of the Health 2030 coordination team, alongside Didier Trono and Denis Hochstrasser, vice rector of the University of Geneva and head of the Department of Genetic and Laboratory Medicine at the Geneva University Hospitals (HUG). This large-scale project was initiated in 2015 by the University of Lausanne (UNIL), the University of Geneva, the Swiss Federal Institute of Technology (EPFL), Lausanne University Hospital (CHUV) and Geneva University Hospitals (HUG). Philippe Moreillon has referred to the cooperation, extended this year to Bern, as “remarkable”. “It’s one of the rare projects that combines all the expertise in Western Switzerland.”
Bringing together top experts
The project aims to pool the financial resources and develop the know-how needed to build powerful and efficient personalised medicine tools. The best genomics experts will work together at a sequencing centre located in Geneva and designed by HUG and EPFL, where DNA samples from the entire region—and beyond—will be centralised.
Another centre, likely to be set up in Zurich, will be responsible for proteomics, the study of proteins (gene expression, or proteins, must be looked at to understand what differentiates two organisms with the exact same genes). In 2013, CHUV opened the Lausanne Institutional Biobank (BIL), which already holds the biological samples of nearly 30,000 people, sick and healthy alike, who agreed to donate tissue to research. The BIL will be able to centralise samples from partners and, once the funding is available, these tens of thousands of DNA samples can be sequenced. UNIL will examine epidemiological and ethical issues. “Social sciences —anthropology, ethics, psychology, law and sociology—also play a key role. “Today, we have to evolve towards an interdisciplinary system. And that’s a very positive thing,” says Philippe Moreillon.
Analysing multiple factors
Denis Hochstrasser points out that personalised health is about more than genetics. “This movement has definitely been driven by advances in high-speed genome sequencing, but genetics is just one of the tools used, along with proteomics and metabolomics,” he says. Metabolomics is the study of metabolites, or molecules produced from metabolic processes, present in a cell. “Precision medicine also takes into account all factors that affect a population’s health, including genetics, ecosystems (microbes and toxins) and behaviour (hygiene, diet, physical activity).” If we attach social and emotional variables, such as the family and professional environment and so on, we can easily understand the challenge
faced by doctors and engineers in interpreting these massive amounts of information, commonly referred to as
“big data”.
Cancers and allergies
What will patients actually be getting out of such a massive
cooperation project? With DNA sequencing alone—just one of the techniques used in personalised medicine—applications are immediately available in oncology, says Didier Trono. “We can already stratify therapies, i.e. assign the best treatment based on the tumour’s molecular signature. For example, we no longer diagnose ‘lung cancer’ but analyse the tumour’s mutations, which can be identical in other forms of cancer. This allows doctors
to offer more effective therapies,” he explains. “We can detect the immunological profile of the tumour and target it using immunotherapy. Genetic risk testing is also available, as Angelina Jolie showed the world. The actress underwent a preventive double mastectomy at age 37 after finding out that she carried the BRCA2 gene mutation, which meant that she was predisposed to develop breast or ovarian cancer.”
Allergology is another area where the Health 2030 project
is expected to bring solutions, says Philippe Moreillon. “Allergies are a real public health issue. We’ll eventually be able to expand our scope of action, especially by combining patient data with data from the Federal Office for the Environment.”
And the analysis of those findings can benefit the population in the long term. “One day, when we can inform people—in real time and across all of French-speaking Switzerland—of the concentration of microparticles or detect the presence of allergens and compare that information with local health issues, we’ll be able to act to eliminate the causes. These are all possible applications in the future. All we have to do is develop the know-how,” says Didier Trono.
We are moving towards a clinical-research system in which research will be applied to the clinical experience in near real time. “The challenges are huge,” says Denis Hochstrasser. “We will not only have to balance the technical, medical, ethical and legal issues, but also rethink how we train practitioners and inform patients.” The revolution of our health care system is now. ⁄
A network within a network
The Swiss Personalized Health Network (SPHN) is a national initiative to support personalised medicine. The SPHN aims to “harness the potential of personal health data shared throughout Switzerland, to better manage individual health, disease and research,” says Peter Meier-Abt, president of the Swiss Academy of Medical Sciences, the organisation in charge of coordinating the project through the implementation phase from 2017
to 2020. The Health 2030 programme in Western
Switzerland will participate in the SPHN. “For Switzerland to establish its position in personalised health research, efforts will have to be coordinated nationwide. It will take the involvement of both medical and non-medical partners, including the government, research funding institutions, health care system and industry,” says
Peter Meier-Abt.
Philippe Moreillon is vice dean of the University of Lausanne. He previously worked at CHUV as head of the Antimicrobial Agents Unit, and then at the Infectious Diseases Service. In 2002, he became director of the Institute of Fundamental Microbiology at UNIL.
Denis Hochstrasser, vice rector of the University of Geneva since 2013 and head of the Department of Genetic and Laboratory Medicine, currently oversees operations at Campus Biotech. He is a co-founder of the Swiss Institute of Bioinformatics and scientific founder of the start-ups GeneProt, Genebio and Eclosion.
Didier Trono is a professor with the laboratory of virology and genetics at EPFL. After studying internal medicine and infectious diseases in Geneva in the 1980s, he worked for several years at prestigious institutes in the United States. When he returned to Europe, he headed the EPFL School of Life Sciences from 2004 to 2012.