“In Vivo” met nine experts from CHUV and EPFL who, through their project and experience, embody the alliance between medicine and other sciences.
Stethoscope or algorithm, it’s the same fight

Idris Guessous
Head of the Unit of Population Epidemiology at HUG and registered physician with the Lausanne University Medical Polyclinic
Idris Guessous is convinced that what he learnt as a medical student is not enough to do the best he can at his job. “Individual data don’t explain everything,” says the physician from the Unit of Population Epidemiology at HUG and Lausanne University Medical Polyclinic. "Environmental and contextual factors also play a role in patient health.
But to study those aspects, we need tools other than the ones we have.” After working in general internal medicine at HUG and CHUV and completing a PhD in epidemiology in the United States, in 2013 Idris Guessous set up the work group GIRAPH with Stéphane Joost, a geographical information systems specialist from EPFL. They wanted to better understand how the urban and human environment affects health.
“The two scientific approaches are complementary,” Guessous says. “Even if we come from different fields, we are united by our shared ambition to achieve scientific success.” However, this partnership between doctors and geographical information systems specialists did not take off immediately. It was just the two of them when the project was launched. “But the family gradually grew,” the physician says. “Engineers actually find it very rewarding to work on health data.” This cooperation led the team to unveil in January 2016 a map of Lausanne showing that urbanism and neighbourhood influence obesity. “Doctors should not feel ashamed about seeking help from other experts,” the epidemiologist says.

Lee Ann Laurent-Applegate
Director of the Unit of Regenerative Therapy at CHUV
Lee Ann Laurent-Applegate teamed up with EPFL engineers and biologists to develop the second generation of biological bandages for severe burn victims. Burn wounds are a real nesting ground for microbes. These bandages are unique in that they prevent bacteria from proliferating on wounds and therefore reduce the risk of death due to infection. The technology is based on a biodegradable bandage made of animal collagen and ‘progenitor’ cells that can multiply quickly. “I bring in engineers and biologists every day to the operating room,” says the director of the Unit of Regenerative Therapy at CHUV. “Working with people from different fields is a fascinating experience. It forces us to push ourselves further. I don’t use the same words when I’m talking to a doctor or to an engineer.”
Partnerships between practitioners and experts is nothing new for Lee Ann Laurent-Applegate. Born in the United States, she studied biology in Switzerland after coming to the country in 1989. “In the United States, doctors and other experts – such as engineers and biologists – are used to working in networks,” she says. “Back in those days, we didn’t see that happening in Europe.”
While attending a conference after recently being appointed assistant professor at Baylor College of Medicine in Houston, she met a represen-tative from the Swiss Institute for Experimental Cancer Research. She decided to come back to Switzerland for nine months to work on skin cancer. And she never left.
Grégoire Courtine
Grégoire Courtine’s TED Talk
Neuro-rehabilitation researcher at EPFL
This 41-year old neuroscientist has a background in both physics and medicine. At his laboratories at EPFL, in Lausanne, Geneva and soon Sion and at Suva, he works on spinal cord injuries. A few years ago, the researchers used pharmacological agents and electrical stimulation to help paralysed rats walk again. Grégoire Courtine and his team developed an electrochemical neuroprosthesis that switched the neural network in the spinal cord from a dormant state to a functional state, and a new robotic system to support the rat in any direction. After several months of work, certain connections were rebuilt.
The team refined its algorithms and interfaces to create a more sophisticated system and conduct experiments on primates which showed greater recovery. A platform for humans was also designed to track muscle activity in real time. The first clinical trials are expected to launch this year. They aim to eventually develop therapies to minimise motor impairment for spinal cord injury patients, stroke patients and patients with multiple sclerosis. Grégoire Courtine sees himself as a “conductor who enables people who speak different vocabularies to understand each other.” He strongly recommends drawing on the model of a single geographical location that brings together researchers and doctors from different campuses in the United States, such as Harvard and the University of California, Los Angeles (UCLA). In fact, he personally feels the “break-up” taking place in Lausanne, as EPFL
and CHUV are no longer located on the same site. “We should bring research more to hospitals,” he says.
Patrice Jichlinski
Chief of the Service of Urology at CHUV
The urologist Patrice Jichlinski worked with EPFL researchers for the first time in 1994. He was developing lasers to treat benign prostatic hyperplasia as part of a joint study conducted between EPFL and the urology departments at CHUV and HUG. EPFL took that opportunity to support and strengthen its expertise in the applications and fundamentals of laser-tissue interactions by working with the urology teams from the two university hospitals. Since then, Patrice Jichlinski has continued to develop the potential of alliances between researchers and practitioners. “As early as the 1990s, the hospital encouraged employees to work with the existing research networks,” he says. The chief of the Service of Urology at CHUV teamed up with EPFL researchers again to develop a technique using fluorescence to detect bladder cancer. Their product is now patented.
Patrice Jichlinski, trained entirely in Geneva, has also been chief of the Department of Surgery and Anaesthesia Services since 2012. Today, he continues to work longside researchers, now from UNIL’s Centre for Cancer Research, on immunotherapy for bladder cancer. “Their work is useful to medicine,” the surgeon says. He believes that the devices developed by scientists, especially engineers, enhance medical learning because they expand the range of surgical instruments. All of the joint projects he has worked on have brought conclusive results.
“It all depends on group cohesiveness. If one person is no longer motivated, the entire project can collapse in a short period of time.”

Brigitte Jolles-Haeberli
Director of the Swiss Biomotion Laboratory at CHUV, professor at UNIL and EPFL
Brigitte Jolles-Haeberli studied microengineering at EPFL and holds a degree and PhD in medicine. She became specialised in arthritis surgery in Toronto and in orthopaedic surgery and traumatology in Lausanne. These days, she spends her mornings performing hip and knee replacement surgery and moves on to research in the afternoon. Alongside teaching at UNIL and EPFL, she leads the Swiss Biomotion Lab at CHUV. This laboratory specialises in analysing movement. It is a place where doctors and engineers work together to find ways of delaying arthritis and better treating the disease. The lab’s experts use a variety of cutting-edge techniques, especially virtual reality, to change how people support themselves to relieve arthritis pain.
Brigitte Jolles-Haeberli – with Julien Favre, Charles Baur and Simon Henein – is working on a custom-fit insole designed to shift the points that support the force on the joints and automatically self-adjust over time.
The expert is also working on another innovation set
for launch soon, a “smart” knee implant. The device is fitted with sensors to provide information that currently remains unknown to the doctor. This same technique could eventually be used for hips and shoulders. “Closing the gap between technical and medical expertise makes the unimaginable imaginable,” the surgeon says. She adds a third area, biology, into the mix, which she believes will deepen knowledge by breaking it down to a smaller scale.

Ioannis Xenarios
Director of the Swiss Institute of Bioinformatics
Ioannis Xenarios, 48, completed his PhD with the Institute of Biochemistry and the Ludwig Center for Cancer Research at the University of Lausanne (UNIL) before moving on to postdoctoral work in bioinformatics at the University of California, Los Angeles (UCLA) in the United States. He built the first knowledge base on protein interconnections, which became an international benchmark. He then worked for seven years at Merck Serono, developing algorithms in genomics and proteomics.
Today, Ioannis Xenarios travels between Lausanne and Geneva on behalf of the SIB to manage two groups, Vital-IT and Swiss-Prot. These two groups bring together a total of more than 120 professionals specialised in a wide range of areas. There are bioinformatics experts, doctors, engineers, physicists, genomics experts and mathematicians. “We try to combine the right skills to make our projects feasible,” he says. These projects include a prenatal test without amniocentesis performed using the mother’s blood. This product is now used in Switzerland and recognised by Swiss national health insurance.
The databases developed by the teams overseen by Ioannis Xenarios are important at both local and international levels. (UniProtKB/Swiss-Prot, the global database containing knowledge about all proteins, is used every month by more than 500,000 people worldwide.) When he’s not supervising research projects, Ioannis Xenarios also plays a role in partnerships with industry and academics. He has been working with CHUV on setting up tools used to analyse genetic variations within the population. This project provided the opportunity to teach doctors about the techniques used in bioinformatics.

Reto Meuli
Chief of the Department of Medical Radiology at CHUV
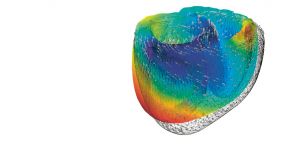
Reto Meuli, 60, is a magnetic resonance imaging expert with degrees in both engineering physics and medicine. He was first confronted with the emerging MRI technology, used to take pictures inside the human body, when he was based in the United States in the 1980s. “With the advances in computer technology, huge progress was made in magnetic resonance techniques between the 1980s and the early 2000s,” he says. “Now the procedure is reaching certain physical limitations. For example, the technology doesn’t require additional computing capacity. Today, one of the main challenges is in functional magnetic resonance imaging, used to measure organ function.” Using fMRI, we can see the brain working and the heart beating or watch a drug’s effect on the body.
Reto Meuli has no doubt about it. “In the years to come, imaging will play an increasingly important role in personalised medicine.” With his training in both medicine and engineering, he can find connections between the needs of patients at CHUV and the findings of engineers at EPFL, who for example work at the school’s Centre for Biomedical Imaging. “My role is to understand and express these needs so that concrete applications can be developed that directly benefit patients.” Meuli believes in the importance of working in line with the philosophy unique to each of the two worlds. He also points out that it is crucial to leave researchers with a bit of spontaneity while taking into consideration the tight financial restrictions.
Olivier Michielin
Physician with the Department of Oncology at CHUV and group leader at the Swiss Institute of Bioinformatics
After studying physics at EPFL, Olivier Michielin, 47, completed a full doctor training programme. He also did his PhD dissertation between Harvard and Strasbourg under the guidance of his supervisor, Martin Karplus, winner of the Nobel Prize in Chemistry for 2013. Together, the two men developed simulation techniques to understand how lymphocytes recognise tumours. Olivier Michielin then took his research in this area forward with his team in Lausanne. “We went beyond understanding recognition mechanisms and modified the receptor in lymphocytes to make them better at recognising tumours.” These “super lymphocytes” have demonstrated their effectiveness on mice. Clinical trials are scheduled to begin in 2017 at CHUV on patients with melanomas. This research could give rise to new treatments for other forms of cancer.
In addition to his work as a doctor, which is how he spends most of his time at the oncology department at CHUV, and in research, which positions him half-way between medicine and molecular engineering, Olivier Michielin is also group leader at the Swiss Institute of Bioinformatics (SIB) in Lausanne. “We’re trying to bring bioinformatics into oncology,” he says. “We’ve only taken the first steps, but it’s one of the key challenges for the future of our discipline. Bioinformatics can be used, for example, to better manage the massive amounts of data to benefit the patient.”

Alain Farron
Chief of the Service of Orthopaedic Surgery and Traumatology at CHUV
Just a few decades ago, orthopaedic surgeons would prepare bones for an implant with little more than the naked eye,” says Alain Farron. “But to keep up with the progress in medicine, these doctors had to find new techniques to prepare the bone site with greater precision.” In a partnership with EPFL and private industry, the chief of the Service of Orthopaedic Surgery and Traumatology at CHUV worked on developing new tools such as 3D printing and computer-assisted surgery to do that. “Bringing engineers to work with orthopaedic surgeons is essential,” Farron says. “We need them as much as they need us.” The doctor works in direct contact with the engineers. Together, they use 3D printing to develop instruments tailored to each patient to find the optimal positioning of implants.
After finishing medical school at the University of Lausanne in 1984 and his post-graduate studies at CHUV and the Cantonal Hospital of Fribourg, he went to work in Philadelphia in 1996. After his experience abroad, he began working with engineers from EPFL. “Relations between the two worlds can be challenging at first,” he says. “But after years of working together, we’ve developed a language we all understand.”
Alain Farron believes that cooperation between engineers and orthopaedic surgeons will grow in the future. He offers
the example of the new Balgrist Campus in Zurich, where engineers develop instruments that surgeons immediately
put to use.
Biotech engineer
These engineers come up
with new materials, forms of
energy or bacteria for the chemical, food, pharmaceutical and other industries. Their inventions are intended to bring solutions to technical issues relating to product design or production.
Digital health
specialist
These experts develop new digital technology to be used in health care. Solutions are designed to help individuals better understand and manage their medical data and allow health care workers to personalise treatments and choose the most effective care strategies for patients.
Bioethics expert
Sometimes called “bioethicists”, they study ethical issues arising from advances in medicine. At a hospital, the bioethics expert could be responsible for determining a patient’s ability to make an informed decision. These experts, employed by the government or an NGO, work to develop ethical health policy.
Medical device
developer
These specialists design innovative instruments and systems to improve or simplify medical procedures. Their inventions, such as medical robots, are used to prevent or treat health conditions and diseases.
Bioinformatician
These computer technology experts build software used to develop drugs, improve quality control in the food industry and protect biodiversity. They analyse researchers’ needs and translate them into computer programmes used in areas such as protein structure modelling and genome annotation.
Diagnostics
technology
developer
These experts come up with techniques for diagnosing new pathologies or simplifying research to identify certain diseases. For example, they may develop cheaper solutions to screen for health problems
in poor countries.